How Long After Achilles Surgery Can I Walk
 By David P. Taormina, MD, and Nirmal C. Tejwani, Doc
By David P. Taormina, MD, and Nirmal C. Tejwani, Doc
Early mobilization and weight bearing after Achilles tendon repair is associated with improved patient satisfaction and faster return to work and sports, with no significant increase in rates of tendon rerupture or postoperative wound and nerve complications.
Achilles tendon pathology can present at whatever age, but epidemiologic studies take shown that men aged between 30 and 50 years are at greatest risk.1 The annual incidence of Achilles tendon rupture is approximately one in 5000 and has increased in contempo decades.2-4 While in that location are well known risk factors, including the use of sure antibiotics (fluoroquinolones5) and steroid injections,6 the archetype history that precedes rupture is that of the episodic athlete—the "weekend warrior."7
When the injury is the upshot of sports action, research has shown that the sport existence played at the fourth dimension of injury varies by geodemographic distribution. In the U.s.a., those afflicted are more probable to take been injured while playing basketball game, lawn tennis, or football game,7 whereas Europeans are more likely to suffer an Achilles injury playing soccer or volleyball.1,2,8 In about of these instances, the deconditioned athlete attempts to perform and exercise at or about their previous level of activeness without accounting for the consequential deterioration of connective tissues associated with crumbling and physical quiescence.
With hyperacute tensile stress across the Achilles tendon, albeit volitional or associated with trauma, sudden plantar flexion or the violent dorsiflexion of a plantar flexed foot forces the largest tendon in the torsonine to the brink of failure. The tendinous bridge betwixt the gastrocnemius-soleus complex (GSC) and the calcaneus is at greatest take a chance for failure at the hypovascular region institute approximately four to six centimeters proximal to its calcaneal insertion.10
Each of the studies the authors reviewed identified advantages of early postoperative mobilization and weight bearing with, at worst, equivocal complication rates
The resultant "pop," which is so often reported by patients, results in the sudden onset of pain, weakness, and difficulty with ambulation. Upon test in the emergency setting or the doctor's role, a lack of plantar flexion forcefulness and unopposed dorsiflexion of the anterior leg musculature, become a main finding on inspection, especially when the patient is lying prone. Confirmation can be made with palpation of a gap between the GSC and heel along with weakness or inability to stand up on one leg. The Thompson test,11 a failure of human foot plantar flexion with a squeeze of the calf, farther confirms the diagnosis. In the rare state of affairs that diagnostic imaging is required,12 magnetic resonance imaging is the modality of choice.
Operative vs nonoperative management
 The war of operative versus nonoperative management for Achilles tendon ruptures has been waged for well over 30 years.13,xiv The debate is fueled on one side past the advantages of surgery for decreasing adventure for rerupture and quickening fourth dimension to render to activity and piece of work. On the other side of the debate, proponents of nonoperative management cite risks of scar adhesion, postoperative paresthesias, and pare sensitivity, and potential sequelae of superficial infections. In fact, these were the study conclusions from a contempo meta-assay by Jiang and colleagues published in 2012.15 Despite an extensive investment of research fourth dimension and a tome-sized plethora of publications, this well-powered review of ten randomized clinical trials, which included nearly 900 patients, establish insufficient evidence to support either operative or nonoperative management.
The war of operative versus nonoperative management for Achilles tendon ruptures has been waged for well over 30 years.13,xiv The debate is fueled on one side past the advantages of surgery for decreasing adventure for rerupture and quickening fourth dimension to render to activity and piece of work. On the other side of the debate, proponents of nonoperative management cite risks of scar adhesion, postoperative paresthesias, and pare sensitivity, and potential sequelae of superficial infections. In fact, these were the study conclusions from a contempo meta-assay by Jiang and colleagues published in 2012.15 Despite an extensive investment of research fourth dimension and a tome-sized plethora of publications, this well-powered review of ten randomized clinical trials, which included nearly 900 patients, establish insufficient evidence to support either operative or nonoperative management.
While the embers continue to burn from a smoldering contend between a prosurgery school of thought and proponents of nonoperative management of Achilles rupture in the full general population, a number of studies have recommended that aristocracy athletes and high functioning individuals undergo percutaneous or open surgical repair for a ruptured Achilles tendon.16-22 The main surgical methods described in the literature are percutaneous repair23,24 through multiple portal incisions, a minimally invasive posterolateral approach25 using a two- to vi-cm incision, and the standard open six- to 18-cm posteromedial arroyo.23
Postoperative rehabilitation
While the literature is rife with publications describing modifications to the documented surgical techniques, this volume of surgical literature is even so eclipsed by the number of postoperative protocol descriptions. Given the contend being resolved between operative versus nonoperative management, it would be ideal to have a postoperative programme that maximizes functional recovery and soft tissue healing while minimizing morbidity, including pain, Achilles rerupture, and associated prolonged hospital form.
The theoretical advantages of early mobilization later Achilles surgery include hastened return of tensile force to the repaired tendon. There is, however, also a hazard for increased rupture end gapping, rerupture, or both. In addition, some other proposed advantage is that early on move prevents germination of adhesions that may ultimately block final range of motion.26
Several studies have described the outcomes of patients who were made nonweight-bearing for half dozen weeks after surgery.27 In fact, a meta-assay performed by Suchak and colleagues included vi randomized trials that compared patients made partial weight bearing on postoperative day 1 versus patients with conversion to weight bearing at three, four, and six weeks postoperatively.27-32 Focusing on rates of Achilles rerupture, subjective patient satisfaction, range of motion (ROM), strength, wound infections, and other minor postoperative complications, their meta-analysis compared a cohort of 315 patients treated with early mobilization (northward = 159) versus late weight bearing (north = 156) afterward operative repair of Achilles tendon rupture.
Ultimately, early functional handling protocols were associated with patients who were subjectively more than satisfied (88% rated postoperative satisfaction as excellent vs adequate or poor) than delayed mobilizers (62% rated satisfaction as fantabulous, p < .0001). There was no statistically significant difference betwixt the rates of Achilles rerupture, which occurred in 2.v% of the early office group and in three.8% of the immobilized patients (p = .47). These rates nearly mirrored the incisional infection rates, as well, which were 2.6% in early mobilizers versus three.9% in the latent mobilizers (p = .63). Finally, assay of an amalgamated variable for other postoperative complications (including sural nerve injury) found that early weight bearing was really associated with significantly lower complexity rates than immobilization (v.8% vs 13.5%, p = .01).27
Studies documenting strength and range of movement after early versus delayed rehabilitation have been less than convincing with regard to recommendations for optimizing patient outcomes. Meta-analysis of available data has shown that early on functional protocols were associated with improved dogie tone and plantar flexion in ane written report, but these findings failed to find back up in the majority of available literature.27 Similarly, advantages in range of move for early rehabilitation accept been supported, at best, inconsistently in the literature.27
Using an creature model (rats), one study has shown that early concrete activity increases the speed of tissue healing subsequently acute Achilles rupture.33 Bring and colleagues used histochemical staining to first identify the postoperative menses of height tissue and nerve regeneration, which occurs between weeks ii and four. Using this information, they then chose the four-week fourth dimension point to compare iii groups of rats that were treated with dissimilar postoperative physical activity protocols: wheel running, plaster treatment, and a control grouping (no strict physical activeness protocol). They found that the wheel-running group did best, showing 94% greater (p = .001) and 48% greater (p = .02) diameter of newly organized collagen than plaster-treated and control rat groups, respectively. Histologic staining demonstrated the wheel-running grouping also had signs of earlier neuronal ingrowth.
A study by our grouping compared the outcomes of 63 consecutive patients who presented with astute airtight Achilles tendon ruptures, 62 of whom had a minimum of half dozen months follow-upwards later existence treated with either minimally invasive open up or standard open surgical repair for an acute Achilles tendon rupture.19
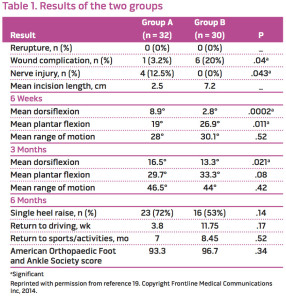
Later surgery, the patient was immobilized in a 10° to 20° equinus splint (minimally invasive group) or removable boot with a 30° heel wedge (standard group) for two weeks. All patients (33 treated minimally invasively, 30 treated with standard open process) were then encouraged to begin weight bearing at ii weeks postoperatively, equally tolerated, with a controlled ankle movement kick fitted with a 20° heel wedge. We theorized that postoperative rehabilitation should be delayed approximately two weeks to allow for the start of early on tendinous fibrous union and to stabilize the soft tissues of the ankle in the postoperative menstruation while incisional wound healing occurred. At half-dozen weeks postoperatively, all patients were converted to a regular shoe with a heel lift. Range of motion, surgical complications (including rerupture and poor wound healing), and sural nerve injury, were assessed postoperatively at the six-week, three-month, and 6-month (with GSC forcefulness assessment) fourth dimension points. The findings are summarized in Table 1.
There were no reruptures identified throughout the postoperative course of the 63 patients. Superficial infections were more than prevalent in the standard open grouping (six patients, xx%) than in the minimally invasive group (ane patient, three%, p = .04). All soft tissue issues resolved without requiring render to the operative suite. Sural nerve deficits were documented in four patients (12.5%) in the minimally invasively treated patients versus none in the standard open up grouping (p = .04). Three of these iv nervus deficits resolved by the vi-month follow-up visit, which raises the suspicion that they were sequelae of traction.
Functional outcomes at final follow-up in 62 patients, using the American Orthopaedic Foot and Ankle Order Scores, did not differ significantly between the groups. Patients had similar arcs of movement during their postoperative course (28° vs 30.1° at six weeks, p = .52) though the minimally invasive grouping had greater dorsiflexion (viii.9° versus two.8°, p < .01) while the standard open group had greater plantar flexion (26.9° vs xix°, p = .01); this may accept been because the well-molded posterior plaster splints positioned the foot in thirty° of equinus (for the open group) versus 10° of equinus (for the minimally invasive surgical group).
Regarding postoperative strength and conditioning, at vi-month follow-upward, we found that 23 patients (72%) in the minimally invasive group were able to perform a single heel enhance (v of the nine who failed to perform heel raise had 4+/v GSC strength), versus 16 of the 30 standard open patients (53%; viii of 14 who failed conditioning testing had 4+/five GSC strength). Although the information trended toward better results with minimally invasive handling, the differences were non statistically significant (p = .14).
The findings of our group go along to support the existing literature on the early rehabilitation of patients later surgical repair of Achilles tendon rupture.34-38 In fact, each of the studies nosotros reviewed identified advantages of early on postoperative mobilization and weight bearing with, at worst, equivocal complexity rates. Furthermore, earlier mobilization was also associated in one study (Suchak et al34) with a quicker return to sports activity and a reduction in the number of lost workdays.
Although inside our report we employed a two-week postoperative initiation protocol for the start of weight-bearing rehabilitation, at that place are other studies promoting partial weightbearing exercises every bit early as postoperative solar day ane.23 Nosotros are unable to document the necessity of a two-week postoperative rehabilitation vacation using scientifically objective findings, but nosotros do subjectively believe there may be a function for an early on postoperative hiatus in order for early on tendinous healing to begin bridging the Achilles rupture gap and for the early progression of the soft tissue healing process.
Decision
The bachelor literature supports, unequivocally, early mobilization and weight bearing in patients after surgical repair of Achilles tendon rupture. Studies have found that early rehabilitation is associated with improved early range of motion. During the early postoperative grade, rehabilitation has been shown to improve patient's subjective ratings of satisfaction, expedite return to work, and allow quicker return to sports activity. When comparing patients with early mobilization to those immobilized iv to 8 weeks postoperatively, there are no differences in Achilles tendon rerupture rates, and similar, or slightly improved, rates of postoperative wound and nerve complications.
David Taormina, MD, is an orthopedic surgery resident at the NYU Langone Medical Center, Hospital for Joint Diseases, in New York City. Nirmal Tejwani,MD, is a trauma fellowship trained surgeon and professor of orthopaedic surgery at NYU Langone Medical Center, Infirmary for Joint Diseases, and at the Bellevue Hospital Medical Center in New York City.
REFERENCES
- Houshian Due south, Tscherning T, Riegels-Nielsen P. The epidemiology of Achilles tendon rupture in a Danish canton. Injury 1998;29(9):651-654.
- Nyyssonen T, Luthje P, Kroger H. The increasing incidence and deviation in sex distribution of Achilles tendon rupture in Finland in 1987-1999. Scand J Surg 2008;97(3):272-275.
- Bhandari M, Guyatt GH, Siddiqui F, et al. Treatment of acute Achilles tendon ruptures: a systematic overview and metaanalysis. Clin Orthop Relat Res 2002(400):190-200.
- Leppilahti J, Puranen J, Orava South. Incidence of Achilles tendon rupture. Acta Orthop Scand 1996;67(3):277-279.
- Huston KA. Achilles tendinitis and tendon rupture due to fluoroquinolone antibiotics. N Engl J Med 1994;331(11):748.
- Kleinman M, Gross AE. Achilles tendon rupture following steroid injection. Report of three cases. J Bone J Surg 1983;65(9):1345-1347.
- Raikin SM, Garras DN, Krapchev PV. Achilles tendon injuries in a U.s.a. population. Foot Ankle Int 2013;34(4):475-480.
- Maffulli N, Waterston SW, Squair J, et al. Changing incidence of Achilles tendon rupture in Scotland: a 15-year study. Clin J Sport Med 1999;9(3):157-160.
- Fornage BD. Achilles tendon: US examination. Radiology 1986;159(3):759-764.
- Jones DC. Tendon disorders of the foot and ankle. J Am Acad Orthop Surg 1993;i(2):87-94.
- Thompson TC. A test for rupture of the tendo achillis. Acta Orthop Scand 1962;32:461-465.
- Garras DN, Raikin SM, Bhat SB, eastward al. MRI is unnecessary for diagnosing acute Achilles tendon ruptures: clinical diagnostic criteria. Clin Orthop Rel Res 2012;470(viii):2268-2273.
- Edna T-H. Non-operative treatment of Achilles tendon ruptures. Acta Orthop Scand 1980;51(6):991-993.
- Wilkins R, Bisson LJ. Operative versus nonoperative management of acute Achilles tendon ruptures a quantitative systematic review of randomized controlled trials. Am J Sports Med 2012;forty(nine):2154-2160.
- Jiang N, Wang B, Chen A, et al. Operative versus nonoperative treatment for astute Achilles tendon rupture: a meta-analysis based on current evidence. Int Orthop 2012;36(four):765-773.
- Bradley JP, Tibone JE. Percutaneous and open up surgical repairs of Achilles tendon ruptures. A comparative study. Am Journal Sports Med 1990;18(2):188-195.
- Karabinas PK, Benetos IS, Lampropoulou-Adamidou One thousand, et al. Percutaneous versus open repair of astute Achilles tendon ruptures. Eur J Orthop Surg Traumatol 2014;24(4):607-613.
- Maffulli N, Longo UG, Maffulli GD, et al. Achilles tendon ruptures in aristocracy athletes. Foot Ankle Int 2011;32(1):9-fifteen.
- Tejwani NC, Lee J, Weatherall J, Sherman O. Acute achilles tendon ruptures: a comparison of minimally invasive and open up approach repairs followed by early rehabilitation. Am J Orthop 2014;43(10):E221-E225.
- Khan RJ, Carey Smith RL. Surgical interventions for treating acute Achilles tendon ruptures. Cochrane Database Syst Rev 2010(9):CD003674.
- Strauss EJ, Ishak C, Jazrawi L, et al. Operative treatment of acute Achilles tendon ruptures: an institutional review of clinical outcomes. Injury 2007;38(vii):832-838.
- Nistor 50. Surgical and not-surgical treatment of Achilles tendon rupture. A prospective randomized study. J Bone Joint Surg 1981;63(3):394-399.
- Gigante A, Moschini A, Verdenelli A, et al. Open versus percutaneous repair in the treatment of acute Achilles tendon rupture: a randomized prospective study. Knee Surg Sports Traumatol Arthrosc 2008;xvi(2):204-209.
- Ma GW, Griffith TG. Percutaneous repair of acute closed ruptured achilles tendon: a new technique. Clin Orthop Rel Res 1977(128):247-255.
- Rippstein PF, Jung Yard, Assal M. Surgical repair of acute Achilles tendon rupture using a "mini-open" technique. Foot Ankle Clin 2002;7(three):611-619.
- Mortensen NHM, Skov O, Jensen PE. Early motion of the ankle after operative handling of a rupture of the Achilles tendon. A prospective, randomized clinical and radiographic study. J Bone Joint Surg 1999;81(vii):983-990.
- Suchak AA, Spooner C, Reid DC, Jomha NM. Postoperative rehabilitation protocols for Achilles tendon ruptures: a meta-analysis. Clin Orthop Rel Res 2006;445:216-221.
- Maffulli Due north, Tallon C, Wong J, L et al. Early weightbearing and ankle mobilization afterward open repair of acute midsubstance tears of the achilles tendon. Am J Sports Med 2003;31(v):692-700.
- Maffulli N, Tallon C, Wong J, et al. No adverse consequence of early weight begetting post-obit open up repair of acute tears of the Achilles tendon. J Sports Med Phys Fitness 2003;43(3):367-379.
- Cetti R, Henriksen LO, Jacobsen KS. A new treatment of ruptured Achilles tendons. A prospective randomized study. Clin Orthop Rel Res 1994(308):155-165.
- Costa ML, Shepstone L, Darrah C, et al. Immediate full-weight-bearing mobilisation for repaired Achilles tendon ruptures: a pilot report. Injury 2003;34(11):874-876.
- Kangas J, Pajala A, Siira P, et al. Early on functional treatment versus early immobilization in tension of the musculotendinous unit later Achilles rupture repair: a prospective, randomized, clinical study. J Trauma 2003;54(6):1171-1180.
- Bring DK, Kreicbergs A, Renstrom PA, Ackermann PW. Physical activity modulates nervus plasticity and stimulates repair after Achilles tendon rupture. J Orthop Res 2007;25(2):164-172.
- Suchak AA, Bostick GP, Beaupre LA, et al. The influence of early on weight-bearing compared with non-weight-begetting after surgical repair of the Achilles tendon. J Os Joint Surg 2008;xc(ix):1876-1883.
- Majewski Yard, Schaeren S, Kohlhaas U, Ochsner PE. Postoperative rehabilitation after percutaneous Achilles tendon repair: early functional therapy versus cast immobilization. Disabil Rehabil 2008;30(20-22):1726-1732.
- Ozkaya U, Parmaksizoglu AS, Kabukcuoglu Y, et al. Open minimally invasive Achilles tendon repair with early rehabilitation: functional results of 25 consecutive patients. Injury 2009;40(6):669-672.
- Twaddle BC, Poon P. Early on motion for Achilles tendon ruptures: is surgery important? A randomized, prospective report. Am J Sports Med 2007;35(12):2033-2038.
- Calder JD, Saxby TS. Early, active rehabilitation following mini-open repair of Achilles tendon rupture: a prospective study. Br J Sports Med 2005;39(11):857-859.
Source: https://lermagazine.com/article/early-weight-bearing-after-achilles-tendon-repair
0 Response to "How Long After Achilles Surgery Can I Walk"
Post a Comment